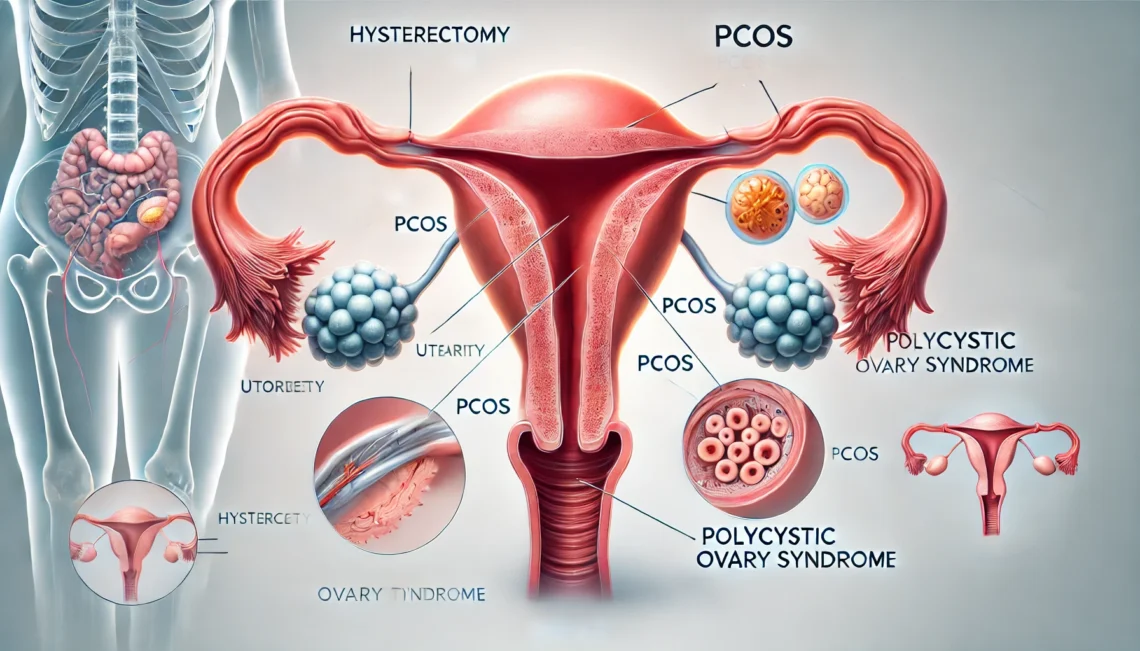
If you’ve been dealing with the ups and downs of Polycystic Ovary Syndrome (PCOS), you might have heard that a hysterectomy could be a potential “cure.” The idea of getting rid of symptoms like irregular periods, acne, excess hair growth, and infertility through surgery can sound tempting. But, is a hysterectomy really the right solution for PCOS? Let’s take a closer look and see what the experts say.
PCOS is a common hormonal disorder that affects women during their reproductive years. It can cause a range of symptoms, including:
- Irregular or missing periods
- Cysts on the ovaries (though not everyone with PCOS has them)
- Insulin resistance, which can lead to weight gain and an increased risk of type 2 diabetes
- Excessive hair growth (known as hirsutism)
- Acne and scalp thinning
- Infertility, as PCOS can disrupt ovulation
While dealing with these symptoms can be frustrating, it’s important to remember that PCOS is different for everyone, and treatment usually focuses on managing the symptoms rather than offering a permanent “cure.” If you’d like to learn more about PCOS, check out this detailed guide from the PCOS Awareness Association.
So, What Exactly is a Hysterectomy?
A hysterectomy is a surgical procedure where the uterus is removed. In some cases, the ovaries and fallopian tubes may also be removed. There are different types of hysterectomy:
- Total Hysterectomy: Removal of the uterus and cervix.
- Subtotal Hysterectomy: Removal of the uterus, but the cervix is left intact.
- Radical Hysterectomy: Removal of the uterus, cervix, parts of the vagina, and surrounding tissues.
While a hysterectomy can resolve certain issues, such as fibroids or chronic pelvic pain, PCOS is primarily a condition that affects the ovaries and hormones—not the uterus. So, removing the uterus doesn’t necessarily address the root causes of PCOS symptoms.
To get a clearer picture of the different types of hysterectomies and why they might be needed, check out this article from Mayo Clinic.
Can a Hysterectomy Cure PCOS?
The short answer: No, a hysterectomy does not cure PCOS. Here’s why:
1. PCOS Is About Hormones, Not Just the Uterus
PCOS is a hormonal and metabolic disorder, which means it affects your ovaries and sometimes your insulin and metabolism. The ovaries in people with PCOS produce too many androgens (male hormones), leading to symptoms like acne, excessive hair growth, and thinning hair. These hormone imbalances are the core issue.
When you have a hysterectomy, you’re removing the uterus, but the ovaries—where the hormonal imbalance starts—are typically left intact. That means your hormone levels may still be out of whack, and you could continue experiencing PCOS symptoms like insulin resistance and irregular periods.
If you’d like to read more about the hormonal causes of PCOS, this fact sheet from the American College of Obstetriciansand Gynecologists can be really helpful.
2. Ovaries Are Often Left Intact
In most cases, a hysterectomy only removes the uterus. Since the ovaries are the main organs responsible for hormone production, leaving them intact means that the hormonal imbalance causing PCOS will likely remain. Even if you have the surgery, you could still deal with symptoms like weight gain, acne, or irregular periods.
In some cases, a doctor might recommend removing the ovaries along with the uterus, especially if there’s concern about ovarian cysts or cancer. However, this would send you into early menopause, which brings its own set of challenges.
To better understand how ovarian removal affects hormone production, you can read this article from WebMD.
3. A Hysterectomy Doesn’t Fix Insulin Resistance
One of the hallmarks of PCOS is insulin resistance, which makes it harder for your body to use insulin effectively. This leads to higher insulin levels, which can trigger weight gain and increase the risk of type 2 diabetes. A hysterectomy doesn’t address insulin resistance or other metabolic issues that are common in PCOS. Without managing insulin resistance with lifestyle changes, medications like Metformin, or other treatments, a hysterectomy won’t help improve this part of the condition.
For more on managing insulin resistance in PCOS, Healthline has a helpful guide.
Why Do Some Women Consider a Hysterectomy for PCOS?
If a hysterectomy isn’t a cure for PCOS, why do some women even consider it? Here are a few reasons:
1. Severe Symptoms
For some women, the symptoms of PCOS can be overwhelming. Issues like chronic pelvic pain, endometrial hyperplasia (thickening of the uterine lining), and heavy or painful periods might push them to consider a hysterectomy. Although these are not typical PCOS symptoms, some women with PCOS develop additional uterine problems, like fibroids or endometriosis, which can make the situation more complicated.
In such cases, removing the uterus can help relieve these specific problems, even though it won’t address the root cause of PCOS. Removing the ovaries might also reduce symptoms like acne or excess hair growth since the ovaries produce the excess male hormones.
2. Family History of Ovarian Cancer
If you have a family history of ovarian cancer or other health concerns, you might consider a hysterectomy (along with ovarian removal) as a preventive measure. However, this is a very specific situation and doesn’t directly relate to PCOS symptoms.
3. Infertility Concerns
Infertility is a major concern for many women with PCOS, and for some, a hysterectomy might seem like a way to “move past” the emotional pain of not being able to conceive. However, it’s important to remember that a hysterectomy removes the uterus but doesn’t fix the hormonal imbalances in the ovaries. So, infertility won’t be addressed by the procedure.
4. A Last-Resort Option
For women with severe, uncontrollable symptoms that don’t respond to other treatments, a hysterectomy may be considered as a last-resort option. But this is not a decision to take lightly and should only be considered after speaking with a gynecologist or endocrinologist.
What Are the Alternatives to a Hysterectomy?
If you’re not ready to undergo major surgery, there are plenty of other treatment options to manage PCOS:
1. Medications
- Birth Control Pills: Help regulate menstrual cycles and reduce acne and excessive hair growth.
- Metformin: Often prescribed to help manage insulin resistance and promote weight loss.
- Spironolactone: Helps block androgens, reducing acne and hair growth.
2. Lifestyle Changes
Regular exercise and a healthy diet can help manage insulin resistance and improve PCOS symptoms. Even modest weight loss can help regulate periods and improve ovulation.
3. Fertility Treatments
If infertility is a concern, options like clomiphene citrate, letrozole, or in vitro fertilization (IVF) can help women with PCOS conceive.
4. Alternative Therapies
Acupuncture, vitamin D supplementation, and herbal remedies have shown some promise in managing PCOS symptoms, though they should be used alongside conventional treatments.
A hysterectomy is not a cure for PCOS. While it can help alleviate certain symptoms, like chronic pelvic pain or fibroids, it doesn’t address the hormonal imbalances or insulin resistance that are at the core of PCOS. If you’re considering this surgery, it’s essential to understand what it will and won’t do for you. Always explore all your treatment options before making such a significant decision.